INside the Mitchell Lab
Crossing Biological Barriers
The Challenge
Solid tumors evade the immune system’s ability to attack them in part due to the tumors’ tough, fibrous biological barriers that circulating immune cells can’t cross. Researchers need to identify ways to deliver individualized treatments that can better target these tumors without causing damage to healthy tissues or affecting overall quality of life.
The Status Quo
Current cancer treatments typically involve surgery, radiation or chemo- therapy to eliminate solid tumors. These treatments are invasive and can cause numerous negative downstream effects. Newer treatments involve engineering a patient’s immune system to recognize and fight cancerous cells, but are so far only effective against certain “liquid” cancers, where the mutated cells circulate freely in the blood and bone marrow and are small enough to be picked off by the patient’s upgraded T cells. Additionally, existing methods can also require that the cell engineering take place in a lab rather than directly inside the body.
Michael Mitchell
J. Peter and Geri Skirkanich Assistant Professor of Innovation in Bioengineering
The Mitchell Lab’s Fix
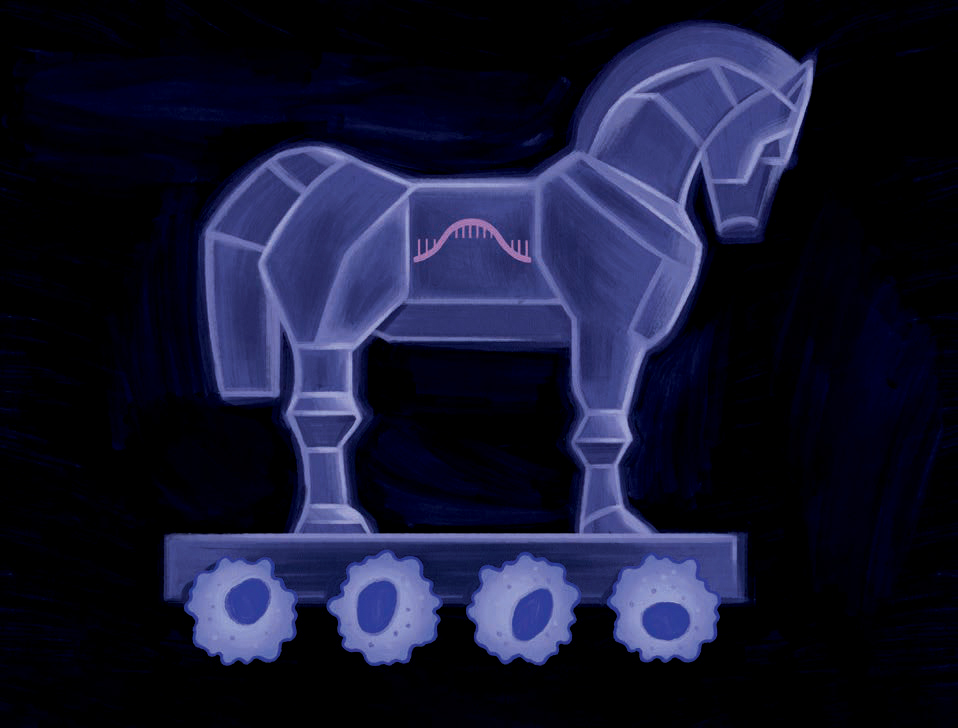
Members of the lab of Michael Mitchell, J. Peter and Geri Skirkanich Assistant Professor of Innovation in Bioengineering, are looking to utilize nanoparticle delivery technology developed by their lab to engineer a different type of immune cell, the macrophage, in order to fight solid- tumor cancers from the inside.
Thanks to the widely publicized technology behind the m RNA -based COVID vaccines, many people know that you can use lipid nanoparticles ( LNP s) to deliver genetic instructions inside a cell in order to get that cell to change the way it functions. In the case of the vaccines, the nanoparticles smuggled m RNA inside of muscle cells in the upper arm to get those cells to produce the spike proteins of the COVID virus, which immune cells could then see, attack and create memory immune cells to fight against future infection with the actual virus.
The Mitchell lab is using the LNP method to carry mRNA and DNA sequences inside of macrophages, a type of immune cell that can consume tumor cells if engineered correctly. In theory, a patient would receive an injection carrying the LNP payload, and the macrophages, whose name literally means “big eaters,” would take up the genetic sequence, alter their function and be able to recognize a patient’s own unique tumor cells in the body.
Because of the way macrophages operate, they could cross the tumor’s biological barrier and attack the cells, destroying the tumor from the inside. An added benefit of the Mitchell Lab’s technology is that the destroyed tumor cells would then also allow other immune cells to present their antigens to circulating T cells, which could then learn to fight those same cancer cells in the future.
In contrast with other engineered macrophage work, scientists using this method would not need to remove the macrophages and engineer them outside the body. The Mitchell Lab’s technology could mean changing the future of solid- tumor cancer treatment from the status quo to one of receiving an injection.
“One of the longstanding challenges that we face in the context of cancer and immunotherapies is that every tumor has unique antigens that are specific to patients,” says Mitchell. “This is why we’ve had a lot of trouble developing targeted therapies. Personalizing an approach by harnessing an individual’s immune system gives each patient a greater chance of a positive outcome.”
Text by Olivia McMahon / Photo by Kevin Monko/ Illustration by Pete Ryan
